How to Tell If You Have a Stomach Ulcer – And Why Early Detection Matters
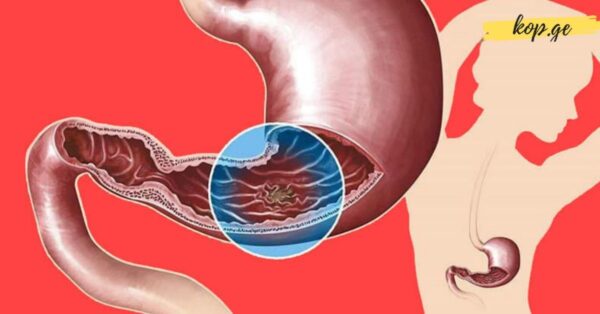
Stomach ulcers, or peptic ulcers, are open sores that develop on the inner lining of the stomach or the upper part of the small intestine (duodenum). Recognizing the signs early can be critical. Left untreated, ulcers can lead to serious complications, such as internal bleeding, infection, or even a perforated stomach lining. Understanding the symptoms and underlying causes can help you seek proper care before the condition worsens.
What Are Peptic Ulcers?
Peptic ulcers come in two main forms:
Gastric ulcers – develop in the lining of the stomach
Duodenal ulcers – occur in the first section of the small intestine (duodenum)
These ulcers are usually caused by an imbalance between the digestive acids in the stomach and the protective lining that shields it. This imbalance often stems from the overgrowth of a bacterium called Helicobacter pylori or from long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or aspirin.
Why Are Stomach Acids Important?
Before diving into the symptoms and causes of ulcers, it’s helpful to understand how your digestive system works.
The stomach is a muscular, sac-like organ located in the upper left part of your abdomen, just beneath the ribs. When you eat, food passes down your esophagus and enters the stomach through the lower esophageal sphincter—a ring of muscle that controls the flow of food. At the other end of the stomach, the pyloric sphincter regulates the flow of partially digested food into the duodenum.
Inside the stomach, special glands produce hydrochloric acid and pepsin, a powerful enzyme that breaks down proteins. A layer of mucus protects the stomach lining from being damaged by these digestive chemicals. If this mucus barrier is compromised—often due to bacterial infection or certain medications—ulcers can form.
Common Symptoms of a Stomach Ulcer
Ulcer symptoms may vary depending on the location, severity of inflammation, and whether there’s a partial blockage in the duodenum. However, some classic signs can alert you to a potential issue:
Mild to Moderate Symptoms:
Burning or gnawing pain in the upper or middle abdomen (often felt between meals or at night)
Bloating or feeling full after eating small amounts
Increased discomfort after eating fatty foods
Nausea or occasional vomiting
Heartburn or acid reflux
Unexplained weight loss
Pain is usually felt in the epigastric region (just below the breastbone), and may improve or worsen depending on food intake.
Severe or Complicated Symptoms:
Vomiting blood or material that looks like coffee grounds
Black, tarry, or bloody stools (a sign of internal bleeding)
Severe, persistent abdominal pain
Shortness of breath or fatigue (linked to anemia caused by bleeding)
Vomiting undigested food due to intestinal blockage
Signs of infection or perforation (fever, rapid heartbeat, sharp abdominal pain)
If you experience any of the above serious symptoms, seek immediate medical attention.
What Causes Ulcers?
Contrary to common belief, stress or spicy food alone doesn’t cause ulcers—though they can aggravate them. Peptic ulcers usually arise from one or more of the following:
1. H. pylori infection
This bacterium disrupts the mucus lining, making the stomach vulnerable to acid damage. It’s one of the most common causes of both gastric and duodenal ulcers.
2. Excessive acid production
Conditions like Zollinger-Ellison syndrome cause tumors (gastrinomas) that stimulate acid overproduction. Though rare, this leads to recurring ulcers that are difficult to treat.
3. Frequent NSAID use
Long-term use of pain relievers such as ibuprofen or aspirin can erode the stomach lining, reducing its natural defenses against stomach acid.
4. Low stomach acid production
Surprisingly, having too little stomach acid (common in older adults or people taking antacids frequently) can also cause problems. Reduced acid can allow harmful bacteria to thrive and interfere with nutrient absorption, weakening the stomach lining over time.
The Role of Stomach Acid in Health
While stomach acid is often seen as a cause of discomfort, it actually plays a vital role in digestion and defense:
Breaks down proteins into absorbable units
Activates enzymes like pepsin
Absorbs key nutrients, including vitamin B12, iron, calcium, and magnesium
Prevents infections by killing harmful bacteria and pathogens from food or drink
When acid production drops due to age or overuse of antacids, several health issues can follow:
Bacterial Overgrowth
Low stomach acid can lead to SIBO (Small Intestinal Bacterial Overgrowth), causing bloating, gas, and inflammation.
Nutrient Deficiencies
Without enough acid, the body struggles to digest and absorb nutrients—leading to deficiencies in iron, B12, zinc, and protein. This can contribute to fatigue, weakened immunity, and even nerve damage over time.
Increased Infection Risk
The stomach is meant to be relatively sterile. Acid acts as a barrier against harmful microbes. When acid levels drop, pathogens are more likely to survive and reach the intestines, disrupting gut flora and overall health.
How Are Ulcers Diagnosed?
If your doctor suspects a peptic ulcer, several tests may be recommended:
Endoscopy – A small camera is used to view the lining of your stomach and duodenum directly.
H. pylori testing – via breath test, stool sample, or biopsy.
Barium X-ray – Less common now but still used to detect ulcers indirectly.
Treatment and Prevention
Treatment typically depends on the cause:
Antibiotics – to eliminate H. pylori infection
Proton pump inhibitors (PPIs) – reduce acid production to allow healing
Antacids and protectants – to ease symptoms
Lifestyle changes – Avoid alcohol, smoking, and NSAIDs when possible. Eat smaller meals and manage stress.
However, long-term use of acid-suppressing medications can come with side effects. It’s important to work with a doctor to identify the root cause and choose the best approach.
Final Thoughts
Stomach ulcers may start as a minor irritation, but they can escalate into serious health threats if ignored. Knowing the warning signs—such as burning pain, bloating, or dark stools—can help you act early. Understanding the role of stomach acid and maintaining a healthy digestive balance through diet and medical care is key.
By being proactive, you can protect your gut, avoid complications, and support your overall well-being.